Congratulations Gary V. Gordon, MD, FACP, FACR, Thomas Harder, MD & Amy Lundholm, DO, Main Line Today’s 2019 TOP DOCTOR WINNERS!
Tag Archives: osteoporosis
New Hours!
To accommodate our patients, Main Line Rheumatology has increased its hours to better serve you!
LANKENAU MEDICAL CENTER
Monday 9am – 5:30pm
Tuesday and Wednesday 8am- 4pm
Thursday 9am – 4pm
Friday 8am- 4pm
MAIN LINE HEALTH CENTER, Broomall
Tuesday, Wednesday and Friday 9am – 4pm
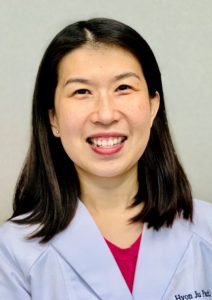
Main Line Rheumatology Welcomes New Staff Rheumatologist, Hyon Ju Park, MD
Philadelphia, PA May 9, 2019… Main Line Rheumatology is excited to announce that we have added Hyon Ju Park, MD, to our staff of rheumatologists. Dr. Park has an impressive resume. She is board-certified in rheumatology and internal medicine, and certified in clinical densitometry (bone density studies). Dr. Park graduated Columbia University in 2003 with a degree in biochemistry, and graduated Mount Sinai School of Medicine in New York, in 2007. She completed a residency in Internal Medicine at Barnes Jewish Hospital in St. Louis, Missouri as well as a rheumatology fellowship and additional research fellowship at Washington University in St. Louis, Missouri.
Dr. Park has been an avid contributor to medical publishing including editorials, reviews, case reports and many book chapters. She has a special interest in lupus, vasculitis, and periodic fever syndromes.
Dr. Park is the mother of two children, and her husband is a cancer researcher at the University of Pennsylvania.
Men Get Osteoporosis, Too!
 Main Line Rheumatology sees many patients with osteoporosis. At least 95% are women, yet statistics looking at people over age 65, find the ratio closer to 50%. Why is that? Most women see their gynecologist for a yearly exam, and those doctors are very good about ordering DEXA (bone density) scans. There is no equivalent for men! Perhaps primary care physicians and urologists should be cautioned that men are at risk for osteoporosis as their testosterone levels fall, just the same as estrogen plummets in women after menopause. Read this informative column by Jane E. Brodey, Personal Health columunist for the New York Times, since 1976.
Main Line Rheumatology sees many patients with osteoporosis. At least 95% are women, yet statistics looking at people over age 65, find the ratio closer to 50%. Why is that? Most women see their gynecologist for a yearly exam, and those doctors are very good about ordering DEXA (bone density) scans. There is no equivalent for men! Perhaps primary care physicians and urologists should be cautioned that men are at risk for osteoporosis as their testosterone levels fall, just the same as estrogen plummets in women after menopause. Read this informative column by Jane E. Brodey, Personal Health columunist for the New York Times, since 1976.
https://www.nytimes.com/2016/10/04/well/live/men-get-osteoporosis-too.html?searchResultPosition=2
Philadelphia TOP DOCTORS 2019 Winners and Still Champions!
CONGRATULATIONS! Philadelphia magazine awards Gary V. Gordon, MD,  FACP, FACR and Thomas Harder, MD, Main Line Rheumatology, TOP DOCTORS 2019!
FACP, FACR and Thomas Harder, MD, Main Line Rheumatology, TOP DOCTORS 2019!
Main Line Rheumatology has offices at Lankenau Medical Center and Main Line Health Center, in Broomall. In addition to Dr. Gordon and Dr. Harder, our doctors, Amy Lundholm D.O. and Hyon Ju Park, MD, are both board certified in rheumatology and internal medicine. Call 610-896-8400 for an appointment. Follow us on Facebook, Instagram and Twitter.
mainlinerheumatology rheumatology philadelphiamagazine topdoctors2019 #drgaryvgordon garyvgordonmd thomashardermd winners
Food and Drug Administration Approves New Osteoporosis Drug That Restores Bone
https://www.nytimes.com/2019/04/09/health/osteoporosis-evenity-bone-amgen.html
The Food and Drug Administration on Tuesday approved an osteoporosis drug, romosozumab (brand name Evenity), that restores bone without breaking it down, according to the findings of two large clinical trials. This breakthrough represents the first new treatment approach in nearly two decades, developed by Amgen, in collaboration with the Belgian drug company UCB. Read more!
Any questions or to speak to one of our doctors, please call 610-896-8400
Did You Know That Certain Medications You Take Can Cause Osteoporosis, Fractures or Bone Loss?
This could be a wake-up call to action!
Glucocorticoids or steroid medications taken for many medical conditions to help you feel better, can end up creating a serious bone fracture and disease problem for many adults. The question to ask yourself, and your family doctor or rheumatologist is, “Am I exchanging one problem for another?”
What are glucocorticoids, and why does my doctor prescribe them, if they lead to bone fractures and osteoporosis? Your body has naturally-occurring glucocorticoids, or steroid hormones, that have many important functions. They help to interrupt or suppress inflammation, help your body respond to stress, and regulate how your body uses fat and sugar.
Many health problems involve inflammation, and if your body’s natural glucocorticoids are not performing well, drug assistance may be indicated. Glucocorticoid drugs are man-made, or synthetic versions of natural glucocorticoids, and can help suppress inflammation from autoimmune reactions, reducing pain, swelling, cramping, and itching. They are prescribed to treat autoimmune diseases like arthritis, rheumatoid arthritis or lupus; skin conditions like psoriasis or eczema; allergic reactions; breathing disorders like COPD and asthma; inflammatory bowel disease like Crohn’s or ulcerative colitis; various cancers, multiple sclerosis; surgery recovery, or sepsis. These drugs are effective in stopping damaging inflammation, but are more potent than the naturally occurring steroids and can cause serious damage.
According to the January 2, 2019 New England Journal of Medicine (NEJM), approximately 1% of all adults and 3% of adults older than 50 years of age receive glucocorticoids for allergies, inflammatory conditions, or cancer. Long-term use of glucocorticoids is associated with clinically significant toxic effects. Fracture, followed by diabetes, is the most common serious and preventable adverse event associated with these agents. The risk of fracture increases with age and with the dose and duration of glucocorticoid use. Here are the facts.
Vertebral fractures are the most common fractures associated with glucocorticoids; the risk of vertebral fracture increases within 3 months after initiation of treatment and peaks at 12 months. The relative risk of clinically diagnosed vertebral fracture doubles and the risk of hip fracture increases by approximately 50% among patients who receive 2.5 to 7.5 mg of prednisolone daily. In a study with a follow-up of 6 months to 10 years, glucocorticoids taken at very high doses significantly increased the risk of vertebral fractures.
Glucocorticoids have direct and indirect effects on bone remodeling. Bone loss can lead to an early increased risk of fracture and osteoporosis. Bone formation also decreases early in glucocorticoid treatment. Indirect glucocorticoid effects predispose patients to reduced muscle mass leading to an increased risk of falls, decreases in renal calcium resorption and levels of sex hormones, and alterations in parathyroid hormone functioning.
The risk of fracture rapidly decreases when glucocorticoids are discontinued. A prospective study showed clinically significant improvement in bone mineral density at the lumbar spine within 6 months after discontinuation of glucocorticoids. A large retrospective study showed an increased risk of a major osteoporotic fracture among patients with recent prolonged glucocorticoid use but not among those with intermittent or past use of these drugs.
What you need to know from this NEJM Report
- Risk factors for glucocorticoid-induced fractures include age (>55 years), female sex, white race, and long-term use of prednisone at a dose of more than 7.5 mg per day.
- Screening for fracture risk should be performed soon after the initiation of glucocorticoid treatment. The risk of fracture among patients who are 40 years of age or older can be estimated with the use of bone mineral density testing and the fracture risk assessment tool (FRAX).
- Patients who receive glucocorticoids should be counseled about adequate intake of calcium and vitamin D, weight-bearing exercise, and avoidance of smoking and excessive alcohol intake.
- Pharmacologic treatment is strongly recommended for anyone who has had a fracture and for patients who are at least 40 years of age if, according to the FRAX tool, the risk of major osteoporotic fracture is 20% or higher or the risk of hip fracture is at least 3%. Among patients who are receiving glucocorticoids and have a bone mineral density T score of −2.5 or less (indicating osteoporosis) at either the spine or the femoral neck, pharmacologic treatment is also recommended for men who are 50 years of age or older and for postmenopausal women.
- Bisphosphonates (i.e. Fosamax, Actonel) are recommended as first-line treatment of osteoporosis because of their low cost and safety.
- The risk of fracture decreases rapidly when glucocorticoids are discontinued. Exposure to glucocorticoids should be minimized as much as possible.
Non-drug options that can help (with or without taking glucocorticoids) bone loss, osteoporosis and fractures
- Weight-bearing exercise, maintenance of normal weight, smoking cessation, limitation of alcohol consumption, and the assessment and management of fall risks.
- Calcium and Vitamin D: Adequate dietary intake of 1,000 mg calcium per day and 600-800 IU of vitamin D (600 to 800 IU) is routinely encouraged in patients who receive glucocorticoids.
- Bisphosphonates increase bone mineral density, help strengthen bone preventing further weakness, and slow down further bone loss.
Be an informed consumer! Talk to your doctor about glucocorticoid drugs that include beclomethasone, betamethasone, budesonide, cortisone, dexamethasone, hydrocortisone, methylprednisolone, prednisolone, prednisone and triamcinolone.
Make every effort to reduce your chance of disabling osteoporosis, fractures and bone loss. Discuss all medication and potential side effects with your primary care doctor, rheumatologist, and/or endocrinologist and together, make the best choices for your overall health and well-being.
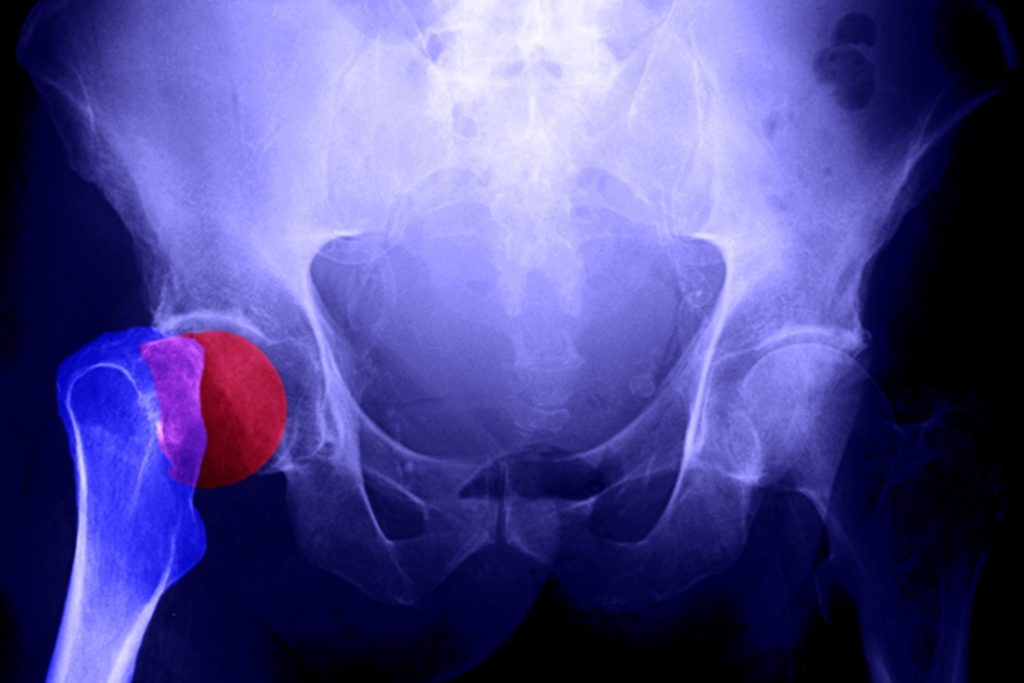
Men and Osteoporosis. It’s Real, and Might Affect You!
To all men over age 50: At your next annual physical checkup visit, ask your doctor to check your height. If you have lost about one inch or more in the past year, you may have male osteoporosis, and is a very noticeable sign.
Osteoporosis is not just a “woman’s disease”. Although osteoporosis is typically 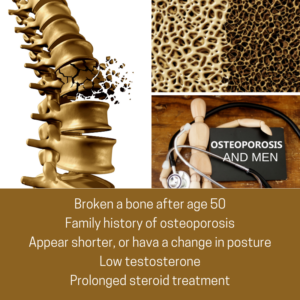 associated with women, it is also diagnosed in men who account for an estimated one in five Americans who have osteoporosis. It is the major cause of fractures in the older population, where bones become thin and brittle, and as a result become weaker and more fragile. Women traditionally experience bone and spine issues after menopause and receive a confirmed diagnosis with a Dexa (bone) scan. However, men are normally not screened for osteoporosis, and don’t learn they have the condition until they experience a fracture. People who have rheumatoid arthritis or who smoke, consume more than three alcoholic drinks a day, have had prolonged prednisone treatment or previously experienced a fracture from only minimal impact should talk to their doctor about starting screening earlier.
associated with women, it is also diagnosed in men who account for an estimated one in five Americans who have osteoporosis. It is the major cause of fractures in the older population, where bones become thin and brittle, and as a result become weaker and more fragile. Women traditionally experience bone and spine issues after menopause and receive a confirmed diagnosis with a Dexa (bone) scan. However, men are normally not screened for osteoporosis, and don’t learn they have the condition until they experience a fracture. People who have rheumatoid arthritis or who smoke, consume more than three alcoholic drinks a day, have had prolonged prednisone treatment or previously experienced a fracture from only minimal impact should talk to their doctor about starting screening earlier.
Be proactive and don’t wait until you experience pain or height loss, before seeking help. Here are some questions to ask yourself.
- Have I broken a bone since age 50?
- Do I have a family history (female or male) of osteoporosis?
- Do I appear shorter, or have a change in posture?
- Do I have low levels of testosterone?
- Do I consume more than three alcoholic drinks every day?
- Have I had any prolonged steroid treatment?
According to a recent article published by the National Institutes of Health (NIH) Osteoporosis and Related Bone Diseases National Resource Center, here is important osteoporosis information for men.
Risk factors linked to osteoporosis in men:
- Chronic diseases affecting the lungs, kidneys, stomach and intestines, or altered hormone levels
- Undiagnosed low levels of testosterone
- Unhealthy lifestyle habits including smoking, excessive alcohol use, low calcium intake, and inadequate physical exercise
- Age: Risk increases with age
- Heredity: A son is almost four times as likely to have low bone mineral density (BMD) if his father has low BMD; nearly 8 times as likely if both parents have it
- Race: All men can develop the disease but Caucasian men at high risk
Osteoporosis can be effectively treated if detected before significant bone loss has occurred. A medical work-up to diagnose osteoporosis includes a complete medical history, x-rays, and urine and blood tests. The doctor may also order a BMD (bone mineral density of DEXA scan) test, which can be used to detect low bone density, predict the risk for future fractures, diagnose osteoporosis and monitor the effectiveness of treatments.
Primary and Secondary Osteoporosis
There are two types of osteoporosis: primary and secondary. Primary osteoporosis is either caused by age-related bone loss (men age 70, and over), or have an unknown cause.
At least half of men with osteoporosis have at least one secondary cause (sometimes more). In cases of secondary osteoporosis, the loss of bone mass is caused by lifestyle behaviors, diseases or medications. The most common causes of secondary osteoporosis in men include exposure to glucocorticoid medication, hypogonadism (low levels of testosterone), alcohol abuse, smoking, gastrointestinal disease, hypercalciuria and immobilization.
Causes of Secondary Osteoporosis in Men
- Glucocorticoid excess (Asthma and rheumatoid arthritis medications)
- Immunosuppressive drugs
- Hypogonadism (Low testosterone levels)
- Alcohol abuse
- Smoking
- Chronic obstructive pulmonary disease and asthma (COPD)
- Cystic fibrosis
- Gastrointestinal disease
- Hypercalciuria (Loss of too much calcium)
- Anticonvulsant medications
- Thyrotoxicosis (Excess thyroid hormone)
- Hyperparathyroidism (Enlarged parathyroid glands)
- Immobilization (Prolonged bed rest or immobilization)
- Osteogenesis imperfecta (Genetic disorder called “Brittle bone disease”)
- Homocystinuria (Metabolism disorder)
- Neoplastic disease (Benign or malignant tumor growth)
- Ankylosing spondylitis and rheumatoid arthritis
- Systemic mastocytosis (Accumulated mast cells in organs)
What You Can Do!
Make an appointment with your rheumatologist or endocrinologist for an evaluation and diagnosis. It’s your continued committed partnership in treating your osteoporosis.
Osteoporosis management includes eating foods high in calcium (i.e. dairy products) and taking vitamin D (1,000 mg daily for men age 50-70; 1,200 mg over age 71), regular weight-bearing exercise, no smoking, limitation of alcohol and caffeine consumption, and fall-prevention.