To all men over age 50: At your next annual physical checkup visit, ask your doctor to check your height. If you have lost about one inch or more in the past year, you may have male osteoporosis, and is a very noticeable sign.
Osteoporosis is not just a “woman’s disease”. Although osteoporosis is typically 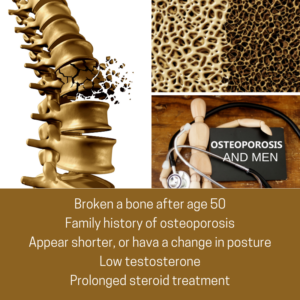 associated with women, it is also diagnosed in men who account for an estimated one in five Americans who have osteoporosis. It is the major cause of fractures in the older population, where bones become thin and brittle, and as a result become weaker and more fragile. Women traditionally experience bone and spine issues after menopause and receive a confirmed diagnosis with a Dexa (bone) scan. However, men are normally not screened for osteoporosis, and don’t learn they have the condition until they experience a fracture. People who have rheumatoid arthritis or who smoke, consume more than three alcoholic drinks a day, have had prolonged prednisone treatment or previously experienced a fracture from only minimal impact should talk to their doctor about starting screening earlier.
associated with women, it is also diagnosed in men who account for an estimated one in five Americans who have osteoporosis. It is the major cause of fractures in the older population, where bones become thin and brittle, and as a result become weaker and more fragile. Women traditionally experience bone and spine issues after menopause and receive a confirmed diagnosis with a Dexa (bone) scan. However, men are normally not screened for osteoporosis, and don’t learn they have the condition until they experience a fracture. People who have rheumatoid arthritis or who smoke, consume more than three alcoholic drinks a day, have had prolonged prednisone treatment or previously experienced a fracture from only minimal impact should talk to their doctor about starting screening earlier.
Be proactive and don’t wait until you experience pain or height loss, before seeking help. Here are some questions to ask yourself.
- Have I broken a bone since age 50?
- Do I have a family history (female or male) of osteoporosis?
- Do I appear shorter, or have a change in posture?
- Do I have low levels of testosterone?
- Do I consume more than three alcoholic drinks every day?
- Have I had any prolonged steroid treatment?
According to a recent article published by the National Institutes of Health (NIH) Osteoporosis and Related Bone Diseases National Resource Center, here is important osteoporosis information for men.
Risk factors linked to osteoporosis in men:
- Chronic diseases affecting the lungs, kidneys, stomach and intestines, or altered hormone levels
- Undiagnosed low levels of testosterone
- Unhealthy lifestyle habits including smoking, excessive alcohol use, low calcium intake, and inadequate physical exercise
- Age: Risk increases with age
- Heredity: A son is almost four times as likely to have low bone mineral density (BMD) if his father has low BMD; nearly 8 times as likely if both parents have it
- Race: All men can develop the disease but Caucasian men at high risk
Osteoporosis can be effectively treated if detected before significant bone loss has occurred. A medical work-up to diagnose osteoporosis includes a complete medical history, x-rays, and urine and blood tests. The doctor may also order a BMD (bone mineral density of DEXA scan) test, which can be used to detect low bone density, predict the risk for future fractures, diagnose osteoporosis and monitor the effectiveness of treatments.
Primary and Secondary Osteoporosis
There are two types of osteoporosis: primary and secondary. Primary osteoporosis is either caused by age-related bone loss (men age 70, and over), or have an unknown cause.
At least half of men with osteoporosis have at least one secondary cause (sometimes more). In cases of secondary osteoporosis, the loss of bone mass is caused by lifestyle behaviors, diseases or medications. The most common causes of secondary osteoporosis in men include exposure to glucocorticoid medication, hypogonadism (low levels of testosterone), alcohol abuse, smoking, gastrointestinal disease, hypercalciuria and immobilization.
Causes of Secondary Osteoporosis in Men
- Glucocorticoid excess (Asthma and rheumatoid arthritis medications)
- Immunosuppressive drugs
- Hypogonadism (Low testosterone levels)
- Alcohol abuse
- Smoking
- Chronic obstructive pulmonary disease and asthma (COPD)
- Cystic fibrosis
- Gastrointestinal disease
- Hypercalciuria (Loss of too much calcium)
- Anticonvulsant medications
- Thyrotoxicosis (Excess thyroid hormone)
- Hyperparathyroidism (Enlarged parathyroid glands)
- Immobilization (Prolonged bed rest or immobilization)
- Osteogenesis imperfecta (Genetic disorder called “Brittle bone disease”)
- Homocystinuria (Metabolism disorder)
- Neoplastic disease (Benign or malignant tumor growth)
- Ankylosing spondylitis and rheumatoid arthritis
- Systemic mastocytosis (Accumulated mast cells in organs)
What You Can Do!
Make an appointment with your rheumatologist or endocrinologist for an evaluation and diagnosis. It’s your continued committed partnership in treating your osteoporosis.
Osteoporosis management includes eating foods high in calcium (i.e. dairy products) and taking vitamin D (1,000 mg daily for men age 50-70; 1,200 mg over age 71), regular weight-bearing exercise, no smoking, limitation of alcohol and caffeine consumption, and fall-prevention.

My uncle was having a hard time moving around because of rheumatoid and he wants to be relieved. It was explained here that the risk involved with bone problems increases with age and needs to be diagnosed early. Moreover, it’s recommended to go to a trusted rheumatologist for quality services.