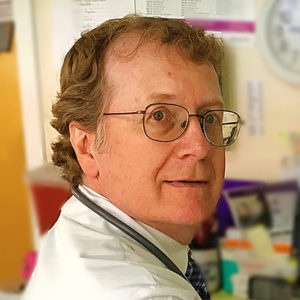
Main Line Rheumatology’s Gary V. Gordon, MD, FACP, FACR and Thomas Harder, MD have been named 2018 “Top Doctors” by Philadelphia Magazine and Main Line Today Magazine. Also Amy Lundholm, DO was named a 2018 “Top Doctor” by Main Line Today Magazine.
Dr Gordon was awarded “Top Doctor” by Philadelphia Magazine for years 2018, 2016, 2015 and 2014, and by Main Line Today Magazine for years 2018, 2017, 2016, 2015, 2014 and 2013.
Dr. Harder was awarded “Top Doctor” by Main Line Today Magazine for years 2018, 2017, 2016 and 2015.